 The debate about death with dignity needs the wisdom of the Catholic spiritual tradition, says this physician and bioethicist.
The debate about death with dignity needs the wisdom of the Catholic spiritual tradition, says this physician and bioethicist.
If you’ve never had to make an end-of-life decision for a loved one, you probably will one day. Eighty percent of hospital deaths now involve an explicit decision to stop some form of treatment. When you make this decision, your stress level will be the equivalent of someone whose house just burned down. And if you’ve never actually talked to your loved one about how they want you to make that decision, your chances of correctly guessing what they want is only two out of three.
Startling facts such as these roll off the tongue of Dr. Daniel Sulmasy, O.F.M. as casually as another doc might say, “Take two aspirin and call me in the morning.” One of the nation’s premiere bioethicists, Sulmasy wears a number of hats in his work at the University of Chicago: Along with being a physician who sees patients and an ethics professor, he teaches in the divinity school, and he’s a Franciscan friar.
Known for tackling tough ethical issues, Sulmasy specializes in decisions at the end of life as well as the spiritual dimensions of practicing medicine. Not surprisingly, he thinks those two are inextricably linked.
Lest anyone think that dealing with life-and-death medical issues all day would be a downer, here’s what Sulmasy told the Chicago Tribune on his appointment to the Presidential Commission for the Study of Bioethical Issues: “I have to say not many people have it as good as I do.”
Why should health care providers be a part of the conversation about the spiritual care of the dying?
Because medicine is inherently spiritual. The first healers, the shamans, were both priests and doctors. There’s something very significant about the interaction between a healer and a patient that raises the big questions, although physicians sometimes don’t allow people to ask them: Why me, or why my child? Why am I suffering? What’s the meaning of this?
If we’re committed to healing patients as whole persons but don’t address those kinds of questions, then we’re negligent in our work as physicians. If all I’m doing is giving chemotherapy, I’m missing 99 percent of the picture.
Is there a special connection between Christianity and medicine?
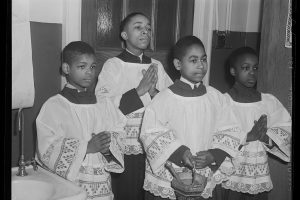
What did Jesus do during his life? He preached and he healed people. Among his first commandments to the disciples is, “Go out and heal people,” and that’s what they do. Read the Acts of the Apostles-it’s all preaching and healing.
For Christians healing has this incredibly special status as an announcement of the kingdom of God. While the miracles of the Old Testament are the parting of seas and pillars of fire, the miracles of the New Testament are healing miracles.
With the advent of early Christianity and even up to the Middle Ages, religion–particularly Christianity–and the scientific medicine of the day are joined. The first hospitals were monasteries. Think of the stories of the St. Bernard dog, going out into the snow and bringing the person into the monastery. The monk-herbalist was the physician. The word hospital comes from the Benedictine virtue of hospitality, of welcoming the sick as guests.
Then with the Renaissance and the Enlightenment, the sense grows that medicine is scientific and religion is superstitious, and that gets in the way of health care. This gradually builds until the middle of the 20th century, when the connection falls apart completely.
Why then?
Partly because medicine became so powerful in the 20th century. Until the advent of antibiotics, doctors couldn’t really do very much for people. But since the 1930s, the advances in medicine have been so astronomical that people look not to God but to the doctor when they’re sick. The doctor begins to think, “I’ve got the power.” There’s this continual suspicion that religion gets in the way of medical progress. When I was in medical school, the patient history form used to ask what the denomination of the patient was. Even that’s disappeared.
Both as physicians and as patients we’ve alienated ourselves from the central meaning of the work by lusting after the technology. We’ve allowed it to be a stumbling block to a truly integrated holistic form of medicine.
So the chaplains go about their work. The physicians go about their work. They’re parallel but not really in concert. For most physicians the work of the chaplain is not really part of medicine. And doctors often think religious people just get in the way–that some fundamentalists will come and ruin our ideas of the best way for this patient to die, or some bishop will tell us that what we want to do scientifically is wrong.
Is there any movement away from the total focus on technology in medicine?
I think both patients and clinicians are experiencing a kind of spiritual bottoming out. The soul seems to have gone out of medicine. Patients feel alienated now by the very progress they were looking for; they feel they’re being treated like machines.
A lot of medical professionals now are saying, if I’m just going to do colonoscopies 20 times a day on patients, I might as well be working in a poultry processing plant. This is not the human experience that both patients and physicians know, in the depths of their souls, medicine actually should be.
I think the inherent contradictions are beginning to dawn on people. Spirituality is being taught in some medical schools now. The number of medical students reporting they feel they have adequate education about death and dying–the time when spirituality comes into play so frequently–steadily increased significantly from the mid-1990s until the mid-2000s.
So how does this all play out in death and dying today?
There are forces going in multiple directions at the same time. On one hand you’ve got people who are denying the reality of death and seeking every kind of treatment. There are physicians who will never stop treating a patient until their very last breath.
On the other side you have people pushing euthanasia and assisted suicide. Ironically, Dr. Kevorkian’s Mercitron machine is actually a child of the same belief in technology, because the solution offered by the advocates of euthanasia and assisted suicide is still based on technology. When the technology of curative medicine fails us, then there will be another technology that can save us–Dr. Kevorkian’s Mercitron machine.
What’s the alternative to “fighting till the end”?
We’re all going to die. Continuing to deny that gets in the way of coming to grips with our humanity and all the important things that we need to do during that period, which can be incredibly rich. Sometimes I enter the room of a patient, and they’re dying in faith and hope and love. I want to take my shoes off before I go into the room. It’s holy ground that I’m treading.
I’m powerfully transformed by that. It’s part of what keeps me in medicine. To see people who really get it, who understand that they’re dying, who are surrounded by people who love them, who care for them. They are dying in love with God, recognize they’re going into the arms of God, and this teaches me about the meaning of my life.
These patients have given a great gift to me, to see that this kind of dying is possible.
What can the Catholic tradition offer the modern approach to death?
From an ethical point of view, it was Catholic theologians 400 years ago who invented the expression extraordinary means. Before bioethics, before machinery, Catholics had been thinking about these questions.
The doctor tells the poor Italian peasant in Sicily that for his health he should go live in the Alps. And the peasant says to his confessor, “I could do that, and it might help me to live longer because the air will be better in the mountains, but I’d bankrupt my family and I’d be separated from them. Do I have to do it?” Before anybody even invented the word autonomy, the wise confessor said, “No, you can take ordinary measures to care for yourself. If something is going to be so burdensome for you as to separate you from your family, then you don’t have to do it.”
In the 1950s that theological machinery was applied by Pius XII to the ventilator. He said, in effect, that Christians have a duty to keep themselves alive, but we recognize that being a good steward of one’s body is a limited duty because the body is limited. Human fulfillment is not in this world, but in the next. So while we have a duty to take good care of ourselves, it is morally permissible to recognize the limits of that and, if something becomes very burdensome, to desist in those kinds of treatments.
What does extraordinary mean in the context of modern medical care?
It is a technical theological term which basically means optional. Antibiotics in certain circumstances can be an extraordinary means of care if they can’t really do much for you. It’s not necessarily how expensive and how many bells and whistles something has, but whether it’s more burdensome than beneficial for the patient.
That moral wisdom is a very significant contribution to better care for the dying, because we need a lot of wisdom now. Eighty percent of patients who die in the hospital now die after an explicit decision not to do something.
This is burdensome. I’ve actually studied this empirically: When family members are asked to authorize not resuscitating a patient, the stress levels are equivalent to somebody whose house just burned down. It is incredibly stressful to be trying to make these decisions.
People feel guilty. I give talks in parishes and people come up to me and say, “Fifteen years ago I told the doctors it was OK not to put my mother on the ventilator, and I always felt guilty about it. I thought maybe I wasn’t being a good Catholic because we’re so pro-life.” I can tell them that our wisdom goes back centuries in being able to say that decision is OK.
Our trust should be in God. We recognize that life is a very important good, but it’s a limited good. You have to die to enter eternal life. That’s central to the Catholic faith. It is death that leads to the resurrection that’s given to us as a gift in Jesus. The Garden of Gethsemane is the human experience. The cup doesn’t pass away from any one of us.
What does a faithful Catholic have to do as a steward of his or her life?
We cannot act with the intention of killing ourselves. But we don’t have to do everything necessary in order to keep ourselves alive. The duty to be a good steward of your body binds up to a point, and then there’s a point at which all of us can say, with St. Paul, I have fought the good fight and I have run the race, I’ve kept the faith, I’ve done enough.
Then I can recognize my dignity, which is the great value that I have.We can, if you will, sin against dignity by trying to prolong life meaninglessly, by not recognizing that our life is finite. That’s why we should stop treatment at the point at which we think it’s more burdensome than beneficial or not really going to be effective.
That’s where the tradition has always been, and I think we need to rediscover that.
Do most people actually talk to their doctors about what they want to do when treatments stop working?
I gave grand rounds (a weekly clinical lecture to a large group of doctors in a hospital) this week on talking to patients or family members about when to stop treatment on their loved ones. One of the oncologists said, “I don’t want to talk to a patient on the first day about these things. But I don’t want to bring it up 20 minutes before they’re dying, either.”
I think doctors err on the side of coming closer to the 20 minutes. You want to give people reasonable expectations about what medicine can do, which is often a lot. But we usually wait too long before we recognize that treatments are failing.
The average time that patients spend in hospice is less than a week. You can have six months in hospice, but often it’s only when someone’s already unconscious that a family member will think that maybe they’re dying and it’s time for hospice now.
Hospice offers an environment where people can really come to grips with some of the spiritual issues in dying. It grew up as a grassroots movement among family members of patients who had died and among nurses, because doctors weren’t dealing with dying well.
What happens when the conversation doesn’t happen?
I have a patient now for whom I’ve basically failed in being able to talk to her and get her to grapple with these issues. She has breast cancer and is in the process of dying.
One of the successes of the technology of medicine is that it’s been able to turn what used to be an acutely lethal disease into a chronic one. Breast cancer used to kill people in a year or two. Now, even with metastatic disease that has spread to different places in the body, people can last 8, 12, 15 years. This patient has had recurrences multiple times, and every time some physician has been able to come up with a treatment to which she’s responded. She’s outlasted all the predictions, 15 years with metastatic breast cancer.
Now the doctor’s bag of tricks is empty, and she can’t believe that it’s possible and is in deep denial. This is getting in the way of her ability to even talk about the possibility of being put on a ventilator, of having her heart stop, and what should be done.
So her faith in the technology has not allowed her to face her own mortality, to deal with the difficulty she’s had with her children and come to reconciliation with that, to help her husband, who wanted to talk to her about planning for her funeral. None of that has been possible because she’s been convinced by the success of medicine that there’s no time that’s going to be the end time for her.
Sadly, the cancer has spread to her brain, and the window of opportunity may have closed for her to do all that spiritual work–what the medievals used to call the ars moriendi, the art of dying. You have to first recognize that you are dying before you can engage in the art.
I faced another situation in which the extent of family denial was so great that an hour after the patient died, family members jumped up on the bed and started trying to do CPR, not once but twice. We finally had to have guards take them away. I mean, that’s absolutely horrific.
Now that person, knowing his children, had appointed a friend to be his health care proxy, and the friend was able to authorize the Do Not Resuscitate order despite the fact that the children were threatening lawsuits.
How do you advise physicians to begin a conversation about dying with a patient or family member?
I teach interns and residents to first use an open-ended statement with family members: “It must be very difficult for you to see your mother, your son, your husband, so sick.” Begin with where they’re at.
Quite often what masquerades as an ethical problem about treatment really is a problem of guilt, anticipated mourning, difficulty in letting go. The doctor needs to establish an empathic connection, recognizing that it’s increasingly burdensome for people because there are all these decisions.
Second is to not be afraid to make a recommendation. I think the pendulum has swung so far in terms of respect for autonomy that people now are abandoned to their autonomy, and that’s a very lonely thing.
We doctors have wisdom. I’ve seen lots of people die. I know how it goes well and I know how it goes badly. I think we should not be afraid to say, Here’s what I think is likely to happen. Here’s what I’d recommend. Now you know your father better than I do. Do you think that’s the right thing for him?
I think that’s better than just asking whether they want us to do this or that treatment. As one of my colleagues has put it, no matter how you ask that question, the family will always hear it as, “Is it OK for Mom to die?”
The correct answer to that question is no. It’s never OK for Mom to die. It may be the right thing, but it’s never going to feel OK. I think we doctors can help people a lot by shouldering some of that responsibility ourselves and making a recommendation rather than making the family think it’s all theirs to do.
Will that solve everything? No. There will be conflicts among family members. And dying people take all their untied endings with them. The doctor can’t fix that. But family members need to try to differentiate between their difficulty in letting go, and what might in the end be what’s really best for their loved one.
Are there particular challenges for Catholics understanding their own tradition?
I’ve had Catholics consistently misinterpreting Catholic teaching. They think they know what the church teaches and they really don’t, so it helps to have somebody who’s an expert tell them, for instance, that we invented the term extraordinary means.
Catholics also need to remember it’s OK to let go. This is maybe not what you’ve heard in sound bites lately on the television. We’re pro-life, but we’re also pro-eternal life, and we have been for centuries, from the beginning.
Related: Do I need an advanced directive?
This article appeared in the November 2010 issue of U.S. Catholic (Vol. 75, No. 11, pages 24-28).
Image: Dr. Daniel Sulmasy, O.F.M; Photo by Meghan Murphy-Gill










Add comment